By Robert L. Moore, MD, MPH, MBA, Chief Medical Officer
“I believe in evidence. I believe in observation, measurement, and reasoning, confirmed by independent observers. I’ll believe anything, no matter how wild and ridiculous, if there is evidence for it. The wilder and more ridiculous something is, however, the firmer and more solid the evidence will have to be.”
– Isaac Asimov, Author and Biochemistry Professor at Boston University
Six years ago, California’s first Surgeon General, pediatrician Dr. Nadine Burke Harris, secured legislative approval to create a supplemental payment for providers to screen adults and children for Adverse Childhood Experiences (ACES) – traumatic events in childhood that can include violence, neglect, abuse, and growing up in a home with substance use and/or mental health challenges. To be able to be paid the $29 reimbursement for screening, clinicians needed to complete a standardized training, which includes some basics on a related topic: trauma-informed care.
The rollout of the ACES screening has been turbulent. However, a moderate amount of screening state-wide has been done, with 29% of the overall Medi-Cal population and 12% of Partnership members having been screened since January 1, 2020. There are different billing codes for low-risk (scoring 0-3 on the ACES screen) and high-risk screening results (scoring 4-10). This allows the Department of Health Care Services (DHCS) to report on the proportion of those who are screened with different risk scores. This year, they reported that 7% of children and 18% of adults had ACES scores of 4 or higher across all Medi-Cal-managed care plans.
The Surgeon General’s program, ACES Aware, also funded several studies and implementation projects. Ostensibly, these grants were supposed to develop an evidence base for the effectiveness of interventions to address ACES and potentially mitigate their effects. In practice, these many studies brought forth many interesting insights, anecdotes, and ideas around ACES and trauma-informed care, but little evidence on outcomes.
One of these studies – which documents a series of interviews of clinicians working in Tribal health centers – notes that the ACES screening tool is not very helpful for Native American populations (Garrow & Wimsatt, 2021). This is because certain kinds of trauma, such as historical trauma, transgenerational trauma, and efforts at cultural erasure, are pervasive undercurrents experienced by our Tribal communities and are not covered in the ACES screening tool. The ACES screening tool was first designed in the late 1990s by Kaiser San Diego for insured adults in an urban setting. The Suscol Intertribal Council offers an excellent online course that encompasses the vital nature of California’s history through the lens of our California Tribes and the effects of colonization through the Native American Historical Trauma and Traditional Healing Project.
Despite the lack of studies showing benefits of ACES screening, ACES Aware and the DHCS websites both authoritatively assert that ACES screening is a vital component of addressing underlying trauma. In addition, DHCS considers ACES screening as an option for a standardized risk assessment expected to be performed by primary care providers on their patients, evaluated as part of the triennial Partnership Medical Review process.
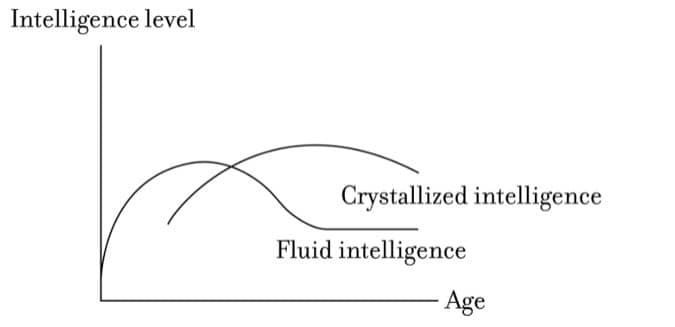
The other options are routine screening for Social Determinants of Health and performing a standardized cognitive health assessment for members aged 65 and older.
Other national organizations are more skeptical. The US Preventive Services Task Force and the Cochrane Collaborative have no recommendations about ACES screening or trauma-informed care. These organizations have endorsed screening for intimate partner violence and depression based on evidence screening, which can lead to interventions and improve outcomes. In January 2022, American Academy of Family Physicians (AAFP) recommended a “universal precautions” approach to trauma-informed care with no screening requirement:
“Providing trauma-informed care does not require individuals to disclose their specific trauma history. Family physicians should approach trauma-informed care itself as a universal precaution by utilizing trauma-informed practices in all patient interactions, even if a patient’s experiences with trauma are unknown. The AAFP urges its members to understand and incorporate trauma-informed care into clinical practice.”
In an effort to review the evidence base more systematically, the US Agency for Healthcare Research and Quality commissioned a study sponsored by the National Institute of Health, released in 2025, titled “Trauma Informed Care: A Systematic Review.” A summary of this study can be found in the November edition of the American Family Physician Journal, Trauma-Informed Care: Evidence and Pragmatic Approaches on page 474.
The summary found that the studies that were reviewed had a high risk of bias and high variability of interventions. The studies were not structured to disprove the null hypothesis: that ACES screening and trauma-informed care have no effect. Partly for this reason, the investigators concluded, “the evidence was insufficient to reach any conclusions about the effects of trauma-informed care for any outcome (Nguyen-Feng, et. al, 2025, p. 9).”
Of course, the absence of evidence is not the same as evidence that something doesn’t work. However, the amount of money and effort dedicated to a particular intervention deserves to be linked, at least somewhat, to the level of evidence behind that intervention.
In the last decade, it seems many well-intentioned researchers who believe a particular fact have been negligently unaware of how their biases affect their study design and validity. Economist Ronald Coase once said, “If you torture the data long enough, it will confess.” Following this logic, we cannot insist on “following the evidence” for the effectiveness of vaccines and the safety of acetaminophen in pregnancy, for example, while following a different standard about interventions that address the important issue of ACES screening and trauma-informed care.
With the absence of outside studies showing a benefit, I encourage you to consider analyzing your own experience. If you are regularly performing ACES screening, consider gathering your own data on the follow-up of this screening. If positive outcomes are being observed, understand the sequence of activities that led to these outcomes. If you find unintended negative consequences, embrace the opportunity to dive deeper into the drivers of these consequences. Make every effort to follow the data to whatever conclusions they reveal.
In the meantime, the AAFP-recommended approach – assuming that any given patient may have trauma impacting their care experience – of providing universal trauma-informed care seems patient-centered and sensible (although this too is not rigorously supported by evidence). The benefit of universal ACES screening itself remains unproven, although perhaps learning about the association between a high ACES score, chronic disease, and poor health outcomes can help motivate our teams to study and understand the principles of trauma-informed care more diligently. Additionally, the $29 per screening in supplemental income from universal screening can help subsidize counseling and staff education around trauma-informed care.
To conclude, I leave you with some final words of wisdom on this topic by Partnership medical director and family physician Dr. Marshall Kubota:
“Maybe it’s the long-term relationships that family physicians (and other primary care physicians) develop over time with their patients (past trauma and other life events) that inform us as doctors, that are threatened by the lack of continuity and time with patients, and cannot be replaced by AI. On the other hand, I don’t know if we can ever really know our patients that well. We might be fooling ourselves that a questionnaire or trauma history would give us the sympathy/empathy that would be needed, especially as it is transmogrified by our own personal history and culture.”

 y change and implement local initiatives to meet the maternity care needs of rural communities. The stakeholders include:
y change and implement local initiatives to meet the maternity care needs of rural communities. The stakeholders include: