The Case for Advance Care Planning. Advance care planning is a series of conversations that a patient and you, their care provider, have about end of life wishes. Continue reading
Monthly Archives: December 2017
When to Consider Palliative Care/Hospice for Patients with Advanced Dementia
Written by: Scott Endsley, MD, MSc., Associate Medical Director for Quality
Dementia is a terminal illness, like cancer or advanced heart disease. Dementia is rapidly increasing in the U.S. and worldwide. In 2012, there were over 5.2 million Americans with Alzheimer’s Disease (AD). By 2025, the number is expected to grow by almost 30% to 6.7 million.[1] Along with the prevalence expanding at epidemic proportions, mortality also continues to increase. It is the 5th leading cause of death in the U.S.[2]
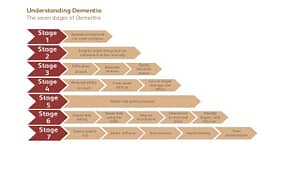
Dementia is a progressive disease with seven stages (figure 1). Alzheimer’s Disease may last for decades, though the mean in eight years. The Global Deterioration Scale[3] is a validated instrument that is helpful in staging the patient along the progression timeline. Memory and function loss proceeds inexorably across the stages until Stage 7 in which the patient has very limited words, incontinence, severe function loss requiring assistance for ADLs, and total disorientation. Median survival in Stage 7 is 1.3 years. Over 80% of patients in this stage have significant eating problems, often requiring assistance. Resultant weight loss is common. Infections, primarily pneumonia and urinary tract infections, are common and carry a high risk of mortality (40% or greater in the CASCADE study[4])
Palliative care is appropriate at any point after diagnosis and may be provided along with symptom management as early as Stage 2. Caregivers and providers are often confronted with the agonizing decision of anticipating death and entering the patient into hospice. Prognostication in advanced dementia is a problematic endeavor. The ADEPT tool has been developed to assist in predicting survival based upon eleven variables in demographics, cognitive status, functional status, active diagnoses. Risk scores greater than 16 (scale 1-32) suggests a six month probability of dying of > 50%. The Medicare Hospice guidelines requires the patient to have significant functional limitation (Stage 7 or beyond of Functional Assessment Staging (FAST) scale) AND at least one of six medical complications in the preceding year including aspiration pneumonia, pyelonephritis, septicemia, multiple decubitus ulcer, recurrent fevers after antibiotics, or inadequate hydration and caloric intake with 10% body weight during previous 6 months (or serum albumin less than 2.5 g/dl). When compared to the ADEPT prognostic tool, the Medicare Hospice guidelines perform less reliability in predicting 6 month mortality.
Recommendations. As your patients with dementia of any type (Alzheimer, vascular, Lewy body) progress through the seven stages, consider the following:
- Educate caregivers on the nature of dementia as a progressive and ultimately fatal disease
- Initiate advance care planning conversations early (stage 1 or 2)
- Ensure that a surrogate has been identified to medical decision making
- Start palliative care in addition to other medical care early or at least by Stage 5 or 6.
- Manage symptoms (neuropsychiatric, incontinence, insomnia) appropriately
- Recommend caregiver assistance early to avoid burn-out and depression
- Consider hospice evaluation at Stage 7
Resources. Many dementia management resources are available. Consult these as needed.
Alzheimer Association: www.alz.org
National Institute for Aging: www.nia.nih.gov/health/alzheimers-dementia-resources-for-professionals
National Hospice and Palliative Care Organization: www.nhpco.org/resources-access-outreach/dementia-resources
[1] Alzheimer’s Association. 2012 Alzheimer’s disease facts and figures, accessed at: www.alz.org/downloads/facts_figures_20122.pdf
[2] Tejada-Vera B. “Mortality from Alzheimer’s disease in the United States. NCHS Data Brief. National Center for Health Statistics, Hyattsville, MD 2013
[3] Reisberg B, Ferris SH, de Leon JJ, Crook T. “The Global Deterioration Scale for assessment of primary degenerative dementia”. Am J. Psychiatry (1982), 139: 1136
[4] Mitchell SL, Teno JM, Kiely DK et al. “The Clinical Course of Advanced Dementia”, NEJM, (2009), 361:1529
What to Know but Not Forget About Dementia
CASE: One of your patients brings in her mother who she reports is having increasing forgetfulness. She is 82 years old, with longstanding hypertension and heart disease. No history of stroke. The forgetfulness was starting to be noticed in her late 60’s and has progressed gradually since then.
Does this patient have dementia? The Alzheimer’s Association recommends looking for the ten warning signs of dementia that include:
- Memory loss that affects daily living or work
- Difficulty performing familiar tasks
- Problems with language
- Disorientation in time and space
- Poor or decreased judgement
- Problems with abstract thinking
- Misplacing things
- Changes in mood or behavior
- Changes in personality
- Loss of initiative
Dementia is very common, affecting up to 50% in patients over 85 years of age, and 10% in patients 65 years. As we all age, our memories decline. However, primary care physicians should be alert to patients who are experiencing memory loss without other signs of cognitive impairment. This is defined as mild cognitive impairment (MCI). Unfortunately up to 81% of patients who meet the criteria for dementia never receive a documented diagnosis. Up to 25% of patients with MCI progress to full dementia each year, and should be evaluated and managed.
Key diagnostic studies include a CBC, serum glucose, serum electrolytes with BUN and creatinine, serum B12 levels, liver function tests, thyroid screening with TSH and depression screening. The latter is crucial as many patients with depression present with mild cognitive impairment. At the present time, there is little evidence to screen for syphilis (unless specific risk factors exist), doing EEGs, APOE genotyping, MR or CT scans or SPECT scanning. Use of PET scans or genetic screening for Tau mutations are controversial.
If cognitive impairment exists, consider use of cholinesterase inhibitors or vitamin E in patients with mild to moderate dementia. Diagnose and treat depression and psychosis as appropriate. Many patients with dementia develop functional or behavioral problems. Consider the following:
- Behavioral modifications (scheduled toileting)
- Music especially during meals and bathing
- Walking or light exercise
- Pet therapy (yes with animals, not electrons)
- Cognitive exercise