By Robert L. Moore, MD, MPH, MBA, Chief Medical Officer
“The waves are going to keep coming, so you might as well learn to surf.”
— Jon Kabat-Kinn, PhD, Founder of Mindfulness-Based Stress Reduction
Partnership data from 2024 showed a significant drop in Influenza vaccination in adults and children, representing part of a larger national trend. Partnership clinicians report an increased hesitancy to receive the flu vaccine, somewhat associated with residual concerns about the COVID vaccine, is the major driver for this decrease.
Since the beginning of 2025, Influenza has overtaken COVID as the major cause of hospitalization and death from respiratory disease, as seen visually in the graph below. In the first week of February, there were three times as many deaths from influenza as from COVID in California, and four times as many hospitalizations. In California, 11 children died due to influenza over the last past seven months; three children died of COVID during the same period.
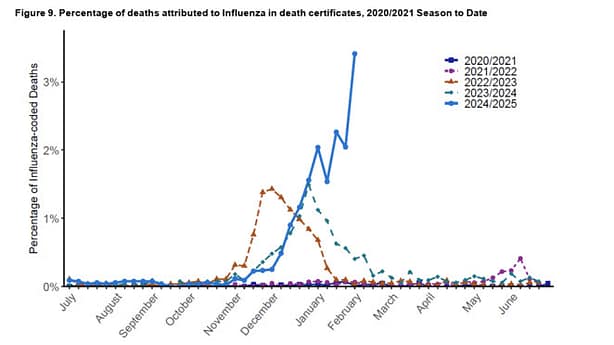
Source: California Department of Public Health
The low vaccination rate, combined with a less-exact match of the vaccine to the currently circulating strains of influenza, are contributing factors to this increase in influenza concerns. While hospitals and emergency rooms are especially busy, there have not been widespread cancellations of elective surgeries; emergency room diversions and patients boarding in areas not usually used for acute patient care have been far below what was seen at the peak of COVID infections and during the H1N1 influenza pandemic of 2009.
Amid the spread of influenza, bird flu (H5N1) is ravaging chicken farms leading to occasional infections of agricultural workers in the dairy and poultry industries. Fortunately, the bird flu strain appears much less virulent for humans than the Influenza A currently circulating.
Strategies for Addressing Influenza Vaccine Hesitancy
- De-couple messaging about influenza vaccine recommendation with the recommendation for COVID vaccination booster infection. Instead of recommending COVID and Influenza and getting a “No” for both, look at the patient history of vaccination and vaccine hesitancy to customize your recommendation. Depending on the pattern, you might try recommending influenza alone or a combination of vaccinations, i.e. RSV and influenza, or pneumococcal and influenza.
- Discuss the current high rates of influenza hospitalization and death to make the case for getting vaccinated. This year’s influenza vaccine can still be given, and it is particularly important for children younger than 24 months who have not completed their primary series of two influenza vaccinations. Remind parents that vaccinating children against influenza helps keep them healthy and provides better outcomes for a full recovery.
- Set realistic expectations: The CDC recommends framing the flu vaccine as a vaccine for the reduction of the severity of influenza, not complete prevention. If patients believe the vaccine is supposed to prevent all infections, they will lose faith in vaccinations if they contract influenza after getting vaccinated.
Thank you for passing this message along to your clinicians!
