10-Minute Mini Lesson Four: Scheduling Fun, Enjoyment, and Achievement
10-Minute Mini Lesson Four is designed to provide a basic understanding of how to help members set schedule fun, enjoyment, and achievement as part of their pain management treatment.
IS LAUGHTER THE BEST MEDICINE?
For years, humor has been used in medicine. Surgeons used humor to distract patients from pain as early as the 13th century. Later, in the 20th century, came the scientific study of the effect of humor on physical wellness. Many credit this to Norman Cousins. After years of prolonged pain from a serious illness, Cousins claims to have cured himself with a self-invented regimen of laughter and vitamins. In his 1979 book Anatomy of an Illness, Cousins describes how watching comedic movies helped him recover.
Over the years, researchers have conducted studies to explore the impact of laughter on health. According to some studies, laughter therapy may provide physical benefits, such as helping to:
- Boost the immune system and circulatory system
- Enhance oxygen intake
- Stimulate the heart and lungs
- Relax muscles throughout the body
- Trigger the release of endorphins (the body’s natural painkillers)
- Ease digestion/soothes stomach aches
- Relieve pain
- Balance blood pressure
- Improve mental functions (i.e., alertness, memory, creativity)
Laughter therapy may also help to:
- Improve overall attitude
- Reduce stress/tension
- Promote relaxation
- Improve sleep
- Enhance quality of life
- Strengthen social bonds and relationships
- Produce a general sense of well-being
Today more than ever before, people are turning to humor for therapy and healing.
FIVE EXERCISES FOR LAUGHTER THERAPY:
- Humming Laughter Sounds: Laugh as you hum, mouth closed. Play with the pitch, up and down the scale, feeling the vibrations resonate through your body. As you get more adapt at feeling the resonation, try and move it deliberately, through your chest, your jaw, your nose, your sinus cavities, your forehead, the top of your head, then back down again.
- Laughter Breath: Inhale deeply, and then exhale in a combination of first quick bursts of air coming out and finishing with vocal laughter. Repeat 5-7 times.
- Laughter Vowels: Laugh the sound of the following laughter vowels. Let’s start with: “A” as in “papa”: Aaaaa ha ha ha ha ha. Then “E” as in “free”: Eeeee he he he he he. Next is “I” as in “pie”: iiiii hi hi hi hi hi. Next is “O” as in “Bingo”: Ooooo ho ho ho ho ho. Last is “U” as in “soup”: Uuuuu hu hu hu hu hu. Excellent! Now repeat, but backwards.
- Happy Memories Chuckle: Go back in time and find a truly happy memory, typically of a time when you felt safe, loved, surrounded by people you loved, and when you all laughed. Take time to connect with this memory, laughing now as if you were back then. It normally takes 90-120 seconds to start to recreate the associated emotions.
- Hearty Laughter: Make an elongated “aeeee” sound as you slowly lift both arms all the way up, and then laugh heartily with your hands pointed to the sky. Imagine that your laughter is coming straight from your heart.
HOW TO ENJOY LIFE IN SPITE OF PAIN:
Suggestions from real patients at HOW TO COPE WITH PAIN:
I know the pain was going to be there but if I could get out and go places and do things I could still have some kind of life. My husband got me a mobility scooter. I am still restricted as to when I can get out but I do get out.
It is very difficult to maintain a positive attitude when all you feel is pain. Continue everyday being positive and keep going your family and friends need you. Breathe. Exercise. Pray. Diversions. Win your pain battle every hour.
I have a couple hours of the day when I can do a little bit and try to take advantage of cramming fun stuff into those few minutes here and there.
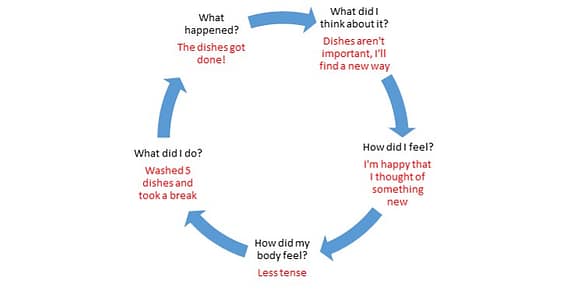
SUGGESTIONS FOR FINDING NEW WAYS TO MEASURE ACHIEVEMENT:
Tell your patients to treasure their big life achievements like graduating from school, getting that promotion, or finding the perfect life partner BUT when battling pain suggest that they DO NOT set that level of accomplishment as a goal.
Instead, they can consider each and every daily life activity as an accomplishment. Here are ten they can start with:
- Waking up
- Brushing my teeth
- Preparing one food item and eating it
- Patting the dog
- Calling a friend
- Typing my own shoes
- Remembering to fill a prescription
- Sitting outside for 15 minutes
- Enjoying a TV program
- Being grateful for the first nine!
*************************************************************************
AS A REMINDER (from the Introduction to this series on CBT for pain management in the primary care office):
CBT is the “gold standard” psychological treatment for individuals with a wide range of pain problems. It can reduce pain, distress, pain interference with activities, and disability. And it may well have positive benefits for common comorbid conditions such as depression, diabetes, and cardiovascular disease. It has been shown to be effective regardless of the particular licensing or background of the provider, as long as they have an understanding of basic CBT concepts and skills, and can even be effective in web-based applications. Brief in-office CBT is not designed to replace referral to a professional mental health provider with his/her diagnostic skills and therapy and/or medication options when this seems more appropriate.
CBT is not just for the licensed behaviorist! These CBT Mini Lessons can be used by:
- The PCP him/herself (using appropriate billing codes to cover the extra 5-10 minutes),
- Office staff such as nurses, medical assistants, behavioral health providers (using Health & Behavior codes billed to PHC)
- A co-located Beacon-credentialed behavioral health provider (billed to Beacon)
Having practiced as a cognitive behavioral therapist for 40 years, I’ve seen CBT techniques used effectively in individual and group settings, in both clinical and psycho-educational venues, and provided by both professional and para-professional providers.
What are the advantages of bringing CBT into the primary care office?
- PCP is best qualified to understand Member’s medical history and current needs.
- Interventions are made when the Member is most motivated for change, i.e., the very moment when they are asking for help
- Providing behavioral alternatives allows the PCP to manage the Member’s pain more safely
- CBT interventions with home practice recommendations and handouts are quite effective in the primary care setting
- Avoid the stigma and wait time sometimes associated with referral to a behavioral health specialist
What are the basic goals for using CBT for pain management?
- Improved relationship with health professional—Member not shuffled off elsewhere, workable alternatives to medication changes
- Increased functional activities—Focus changes from Member saying, “I can’t…” to Member asking, “How can I…?”
- Improved mood and quality of life—Decreased depression, more optimism and self-confidence, less risk of side effects from medication
- Improved symptom control—Better awareness of pain cycles, reducing use of unworkable strategies for managing pain
- Improved self-management—Reliance on self rather than others to provide solutions
- Reduction in unnecessary visits—Reliable self-management options rather than unnecessary appointments when pain increases
By Karen Stephen, Ph.D., PHC Mental Health Clinical Director