By Robert L. Moore, MD, MPH, MBA, Chief Medical Officer
See below for this week’s extensive collection of news and information on COVID-19, curated for topics of interest to primary care providers.
These summaries are being posted as blogs on phcprimarycare.org. We have also posted a draft of our recommendations for re-opening outpatient practices on the blog.
Your team at Partnership HealthPlan is here to help and support you as you adapt to this new medical world we are all now living in!
- Optimizing physical exams conducted by video. Several physicians with extensive experience in providing primary care by telemedicine have posted videos sharing their best practices. Here are some links to some of the ones that are particularly helpful.
- General overviews of best practices:
- “Bedside” manner by video (10 minutes)
- General physical exam (5 minutes)
- Provider directed patient self-exam
- Overview (16 minutes)
- Free CME from Stanford (15 minutes)
- Patient assisted virtual palpation (3 minutes)
- Best Practice on Observation (4 minutes)
- Specific Types of Exam
- Abdominal exam (6 minutes)
- Neurologic exam (20 minutes)
- Musculoskeletal exam (6 minutes)
- Orthopedic exams
- Knee
- Hip and Groin; Sample exam
- Shoulder Exam: flexion, adduction, abduction; preparation for patients before visits
- Neck: range of motion, nerve root compression
- COVID Testing
- Antibody tests covered by PHC and MediCal. MediCal codes (86318, 86328, 86769) are a benefit with an effective date of April 10, 2020. The code for the single step method test is 86318, which has a Medi-Cal rate posted. Rates have not yet been set by the state for the other two tests. We recommend checking the CLIA status of these tests before ordering them to conduct in your office.
B. Caution: Antibody tests using Lateral Flow Assay have variable sensitivity. (From UCSF ID) Researchers in the UK (pre-print) evaluated a panel of antibody-based COVID-19 tests – a novel Enzyme-linked immunosorbent assay (ELISA) in the lab and 9 commercially-developed Lateral-Flow Assays (LFAs) to be used at the point of care. Serum of patients diagnosed with COVID-19 served as the positive controls and serum of patients in UK before December 2019 served as negative controls. ELISA identified COVID-19 IgM or IgG antibodies in 34/40 cases and 0/50 controls, yielding a sensitivity and specificity of 85% and 100%. The sensitivity of ELISA IgG improved to 100% when restricted to patients exhibiting symptoms for ≥10 days. No patients were IgM positive but IgG negative by ELISA. LFA had a sensitivity of 55-70% with a specificity of 95-100%. IgG titers rose for 3 weeks post symptom onset and began to fall by 8 weeks, but remained above the detection threshold. This small study was limited by small sample sizes and has not yet been peer reviewed. Bottom line: This study suggests ELISA is best used to identify COVID-19 exposure 10 or more days following symptoms. Despite being available at point of care, currently available LFAs have variable sensitivity. Whether a positive antibody test to COVID-19 by one of these tests correlates with immunity is not known.
C. Persistent virus shedding associated with lower levels of SARS-CoV2 IgG: persistent infection? A recent report showed that some patients shed viral RNA in stool for a prolonged period after symptoms resolved and viral RNA is no longer detectable in nasopharyngeal swabs. Another analysis from China of a subset with renewed detection of RNA after several negative tests found an association with lower levels of viral-specific IgG. This suggests that a suboptimal immune response is associated with persistent or recurrent infection. More study is needed, but this reinforces caution needed when interpreting positive COVID antibody tests, especially the LFA tests, as noted above.
D. PCR/RNA tests using sputum contain more viral material than Nasopharyngeal swab. This pre-publication summary showcases another option for appropriate settings, and may be collectable via self-collection. This may generate more droplets in collection process, but saves swabs which are often in short supply.
- COVID Epidemiology Updates
- Using COVID RNA tests of sewage for population monitoring. As noted previously, SARS-CoV2 RNA has been detected in stool of many individuals with symptomatic COVID. A recent report found that SARS-CoV2 can infect the enterocytes of the human GI tract, suggesting that virus shedding is directly from the GI tract. Several countries have used RNA detection in sewage to detect COVID-19 infection in a community several days before the first symptomatic cases are confirmed.
According to an article in Nature, several groups are conducting these sewage tests in the United States. One area of development is to look at the RNA load in sewage to estimate community prevalence of infection. KQED reported that ten Bay Area Counties and Shasta County are testing sewage; a separate report indicated that Lake county has conducted tests. In Lake county the sewage tests converted from negative to positive a few days before the first cases were identified and confirmed.
Once a community believes it is COVID-free for a period of time, sewage testing may be able to confirm this, and act as an early warning of the return of COVID to a community. Decades ago, this methodology was used extensively in tracking polio incidence in communities.
B. Heat and humidity of the environment may decrease transmission COVID is spreading quickly around the world in countries with a wide variety of climates. Urban crowding seems to be one of the larger risk factors. Other respiratory viruses have less transmission in the warmer months of the year. This may be partly due to the thicker protective mucous in warmer and moister climates, and partly due to more prolonged indoor exposure to people in cooler weather. An elegant analysis of data from multiple countries suggests that there is some slowing of the COVID doubling rate in more tropical climates compared to more temperate climates. This is a mathematical/epidemiological modelling exercise; it will be interesting follow further data analysis from within the United States. Somewhat suggestive: COVID spread was more rapid and harder to control in the Midwest and Northeastern states which are emerging from winter, compared to states in the West and Southwest.
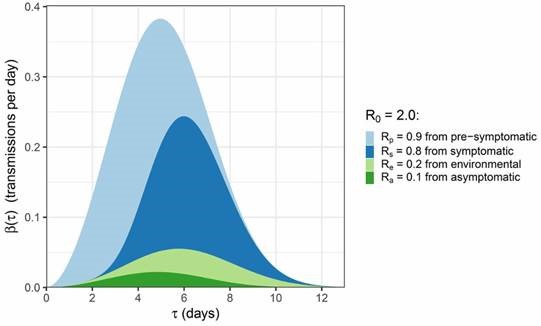
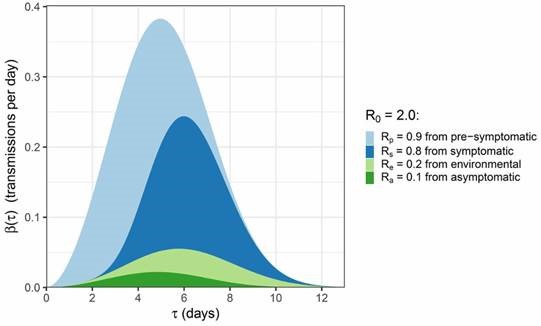
C. Pre-symptomatic infections most infectious. Another complex mathematical analysis of available data published in the journal Science compares the degree and timing of infectiousness in the course of different infection scenarios: pre-symptomatic by droplet/aerosol; symptomatic by droplet/aerosol; by environmental contact (fomites); from asymptomatic individuals. The graphic below summarizes their conclusions: tau represents the time since infection. Again, this is a model; more data will undoubtedly refine it; it reinforces the rationale for population wide facial covering to reduce transmission. I speculate that the decreased infectiousness of symptomatic individuals may be related to greater caution taken in this phase.
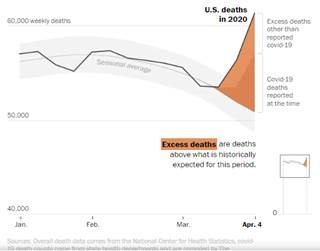
D. Why are mortality spikes greater than can be accounted by reported COVID deaths, in countries around the world? Last week, an analysis of reported mortality data from around the world found that, in many countries, the overall mortality rate increased sharply, but much more than would be accounted for by COVID-reported deaths. A few days ago, a similar phenomenon was reported in the United States, for the last two weeks of March, when COVID deaths accounted for only 53% of excess deaths. Here is the graphic:
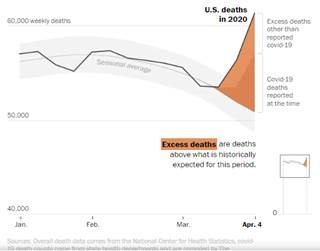
Interestingly, most of these excess deaths were in the Eastern US, the percentage is notably less in Michigan and absent in Washington state. There are multiple possible contributory explanations/factors; more analysis will shed more light on this.
E. COVID deaths outside the hospital (often at home), not counted in official estimates; possibly related to the hypoxia without dyspnea described in a prior update.
F. Strokes in young patients, related to hypercoaguable state induced by COVID infection, which may be due to the recently documented direct infection of endothelial cells by SARS-CoV2, with subsequent damage, promoting thrombogenesis. New York City found a doubling in the rate of strokes in the past month, with half the cases in younger patients infected with COVID.
G. Patients not going to hospital due to fear, dying of heart attacks, strokes, other emergency medical conditions.
H. Increase in suicides. Of note for the first possibility: PHC now covers O2 sat monitors (HCPCS E0445) provided by DME companies. However, due to an international shortage, your local DME vendors may encounter difficulty fulfilling a prescription for an oxygen saturation monitor. PHC is working on an alternative consignment and distribution process for O2 Sat monitors; more to come.
- Updates on therapeutics
- Tocilizumab for reducing cytokine storm. (From UCSF ID) Two recent papers seek to uncover the mechanisms behind the development of acute respiratory distress syndrome (ARDS) in a subset of COVID-19 patients often >7 days after onset of symptoms. Blanco-Mello et al compared the transcriptional response of SARS-CoV-2 to other respiratory viruses including Influenza A in a variety of immortalized tissue culture cells, infection of primary airways cells, in vivo samples derived from SARS-CoV-2 infected ferrets, and finally from post-mortem samples collected from the lungs of humans who died with SARS-CoV-2 or normal lung biopsies. These studies, together with serum profiling in the ferret model, revealed a unique and inappropriate inflammatory response characterized by low levels of type I and type III interferons, elevated chemokines, and elevated Interleukin-6 (IL-6) expression.
Giamarellos-Bourboulis et al compared 28 patients with COVID-19 and ARDS to 26 patients COVID-19 without ARDS. Control groups included patients with 2009 H1N1 Influenza A and patients with community acquired pneumonia-associated sepsis. Some patients with COVID-19 associated- ARDS had macrophage activation syndrome, and most had immune dysregulation characterized by low expression of HLA-DR on a subset of monocytes (CD14 positive) that is triggered by monocyte hyperactivation, excessive IL-6 release, and profound lymphopenia. This pattern is distinct from ARDS-associated bacterial sepsis or 2009 H1N1 influenza. Together, these studies suggest that COVID-19 associated ARDS may be characterized by both a reduced innate immune response coupled with an exaggerated inflammatory cytokine response.
A preprint report of a study of 30 patients with severe, deteriorating COVID pneumonia treated with tocilizumab to block IL-6 eliminated the development of cytokine storm, compared to a matched control group. Larger studies are in process.
B. Alpha-lipoic acid reduces systemic inflammatory response in COVID. α- Lipoic acid (ALA), as an antioxidant, has been confirmed to reduce systemic inflammatory response in patients with acute coronary syndromes, liver transplantation patients, and kidney-pancreas combined transplantation patients. A preprint of a study suggests a benefit in reducing cytokine storm in critically ill patients with COVID. Again, more study is needed.
C. Remdesivir: Gilead announced that their trial of Remdesivir has reached its primary endpoint, which likely means a survival benefit has been found. More information and detail will be coming soon.
- Focus on inpatient care issues with COVID patients. Given the seroprevalence data from Santa Clara (the COVID hot-spot in Northern California), it is likely that over 97% of residents of PHC counties have not yet been infected with COVID-19. There is a strong possibility that we will see an increase in COVID hospitalizations in the future, with recruitment of community physicians to assist with their care. All physicians therefore need to learn the essentials of caring for COVID inpatients. Here are some highlights to help prepare.
A. Free clinical simulation of caring for patient with COVID on general hospital floor. This simulation takes about 15-20 minutes and hits on many highlights of caring for COVID inpatients that are not in the ICU. I highly recommend it. The next three items are elaborations of some themes of this simulation. The subsequent five items relate more to critically ill patients in the ICU.
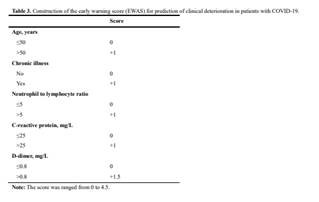
B. Risk factors for deterioration. There are many models for estimating the risk of deterioration. Here is one called the Early WArning Score (EWAS), using just 5 factors: age, underlying chronic disease, neutrophil to lymphocyte ratio, C-reactive protein, and D-dimer levels.
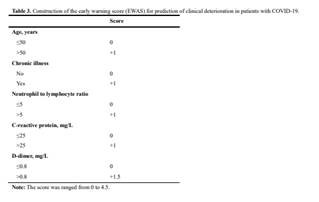
Low risk is a score of 0-2, medium risk is a score of 2.5-3, high risk is a score of 3.5 to 4.5. The 14-day cumulative incidence of clinical deterioration in the low-risk group was 1.8%, which was significantly lower than the incidence rates in the medium- (14.4%) and high-risk (40.9%) groups. Note the heavy weight given to elevated D-dimer level.
C. Aerosolization of COVID with different types of oxygen therapy. The simulation above indicates that less hazardous aerosol is released into the room with a non-re-breather mask than with other high-flow oxygen delivery methods. This study casts some doubt on this popular wisdom, indicating that the aerosolization of all oxygen delivery methods are about the same. Bottom line: wear a tightly-fitting, fit-tested N95 when entering the room of a COVID patient on oxygen.
D. Heparin reduces hypoxia in hospitalized COVID patients. Since we are seeing a variety of blood clots in patients with COVID (strokes, pulmonary emboli, peripheral blood clots), and anti-coagulation is usually beneficial for most hospitalized patients, it is not surprising that this study found improved hypoxia from use of prophylactic heparin in COVID inpatients without active bleeding.
E. The range of survival for ventilated patients varies greatly by hospital/geography: From a survival rate of 12% in New York City to a survival rate of 94% in at San Francisco General Hospital. This is partly related to the effect of an overwhelmed hospital system, in New York, but another factor is the organization of health care delivery at different hospitals. SFGH’s CEO Susan Ehrlich has rigourously overseen the implementation of lean management methods throughout their leadership structure, which led to strong independent, self-improving teams. I would speculate that this is contributing to their amazing outcomes.
F. Outcomes poor for CPR in hospitalized COVID patients with cardiac arrest. This report notes that if patients with COVID get to the stage of cardiac arrest, CPR is unlikely to lead to positive outcomes. Less than 1% of COVID patients receiving CPR survived without permanent neurologic sequelae. This is helpful information for advance care planning conversation.
G. ST-segment elevation in COVID: clot vs. myocarditis? Although the COVID virus infects blood vessel endothelial cells, potentially contributing to blood clots (as noted earlier), this summary found that most patients with ST-segment elevation on EKG are found to have no obstruction of coronary arteries, suggesting that myocarditis from direct COVID infection may be the more dominant underlying etiology, as first noted in Washington state’s experience.
H. Many critically ill COVID patients found to have aspergillus superinfection. This pre-print found Aspergillus in 33% of lung specimens of intubated COVID patients. This might be colonization or superinfection, the latter due to impaired immune response. Evaluating Bronchial secretions of COVID patients for superinfection with both bacteria and fungus seems prudent, to not miss a treatable superinfection.
I. Gut microbiome associated with risk of cytokine storm? Why do some COVID patients become seriously ill, while others do not? This analysis speculates that the proteins produced by the gut microbiome (called the fecal metabolome) may affect the probability of developing cytokine storm. More analysis is needed to understand how this might be leveraged for prevention or treatment.
- What is “Crazy Paving” and what does it have to do with COVID? Crazy paving refers to the appearance of ground-glass opacity with superimposed interlobular septal thickening and intralobular septal thickening, seen on chest High Resolution CT. It is a non-specific finding that can be seen in a number of conditions. Here are two CT scan views showing this pattern, along with a picture of a mosaic paved pathway that inspired this whimsical radiological description.

Crazy paving: not exactly a yellow brick road, but I’ll say goodbye for now.
Robert Moore, MD MPH MBA
Chief Medical Officer