Cancer remains one of the most prevalent and deadly diseases in California as they are in the United States. Nine of fourteen counties served by Partnership exceed the state average prevalence of 417 per 100,000 population; six of the top ten counties in California for cancer prevalence are in Partnership HealthPlan service areas. Breast, colon and lung cancers remain the most common.
Once thought it be primarily relation to tissue destruction and inflammation, with some pain resulting from perineural invasion of the tumor causing neuropathic pain, the understanding of the etiology of cancer pain has shifted to intrinsic pain mediators being secreted by the tumors themselves including the bradykinins, tumor necrosis factors, and granulocyte colony stimulating factors. It’s also known now that cancer induces spinal cord plasticity with overexpression of nociceptive mediators and receptors.
Pain is a very common complication of cancer. Studies have suggested that it is present in over 50% of cancers, with pain ranging from 52% in urogenital cancers to over 70% in head and neck cancers. Yet with all the attention being paid to the opioid epidemic among non-cancer pain patients, the cancer population is not receiving the attention it deserves.
Cancer pain isn’t a single form but has multiple pain syndromes. This is key to identify for each syndrome has different mixes of appropriate management strategies. These syndromes include:
- Pain following procedures/ chemotherapy
- Post-operative pain
- Tumor associated pain (e.g. bone collapse, viscus obstruction, headache, hemorrhage)
- Pain associated with infections
- Nociceptive pain syndromes including paraneoplastic syndromes
- Pain associated with visceral invasion
- Neuropathic pain syndromes
Cancer pain is often accompanied by fatigue and psychological distress. Effective management of cancer pain is complicated by these accompanying symptoms. Some key steps in cancer pain management include:
- Comprehensive assessment- which pain syndrome(s) are present, what is functional and psychological state of the patient, past or current history of opioid use or misuse
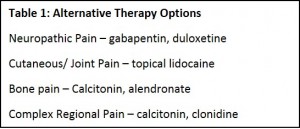
- Therapy Selection – opioids remain the main stay of therapy but consider adjunctive therapies for other types of cancer related pain (table 1). Consider age and end organ function in your selection
- Route – choose the least invasive route such as oral or transdermal
- Dosing – use both basal long acting opioid coverage and use short acting agents for breakthrough pain.
- Monitor effect and side effects closely – use a pain score to evaluate improvement in pain, ask about constipation, sedation, pruritus, and dyspnea. If a particular opioid regimen is not as effective as desired, switch to another type or formulation rather than increasing dose. Treat side effects as they arise.
Consider non-pharmacologic therapies, as well, including acupuncture, massage or TENS.
Monitoring is also very important as the risk of diversion and misuse exists in the cancer population as well as in the non-cancer population. If pain is not being adequately controlled, consider getting a urine toxicology screen to assess compliance with therapy. Use pain contracts as appropriate.
Resources:
- NCCN Adult Cancer Pain Guideline- nccn.org/professionals/physician_gls/PDF/pain.pdf
2. ESMO guidelines – oxfordjournals.org/content/23/suppl_7/vii139.full.pdf+html