By Robert L. Moore, MD, MPH, MBA, Chief Medical Officer
“Change was indeed possible, one person at a time.”
–Mark Bello, Author
The topic of Health Equity is now everywhere: special issues of Health Affairs and JAMA®, legislation, regulatory mandates, etc.
What does it mean for Partnership HealthPlan of California (PHC) and primary care?
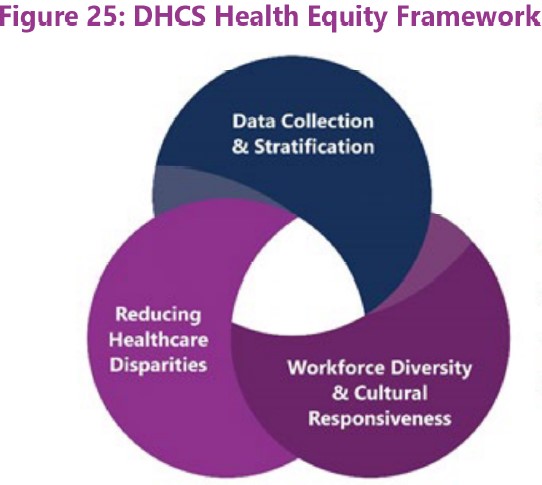
The Department of Health Care Services (DHCS) has a nice framework for thinking about Health Equity (from the 2022 Comprehensive Quality Strategy).
It divides Health Equity into three categories of actions:
- Measurement: Activities related to accurately measuring disparities and inequities. This includes a planned several-year effort to collect Sexual Orientation/Gender Identity information as part of the Medi-Cal eligibility process (in addition to current gathering of race/ethnicity/language data). Overall quality data and outcomes can then be analyzed for each of the demographic groups for which we have data, to look for differences or disparities. These differences may be found at the county, health plan, or provider level, depending on the individual measure characteristics. Example: the rate of BP control is significantly lower for Black men, resulting in increased incidence of stroke and heart attack.
- Interventions: Once disparities or inequities are documented, they can be analyzed to look for drivers or underlying causes. This analysis can then be prioritized into some potential action plans or interventions to close disparities/reduce inequities. There are two major potential causes of confirmed inequities in vulnerable populations:
- Bias/Discrimination. This can occur if a health care professional or support staff make treatment decisions or recommendations based on implicit bias or even explicit assumptions about patients’ values and options, based on their race/ethnicity/language or other trait, and withholds valuable care disproportionately to one group compared to another. Example: Post partum nurses in one PHC contracted hospital don not educate new Latina moms about breastfeeding because they assume that Latina mothers prefer to bottle feed. Provider Intervention: Staff education to understand implicit and explicit bias and learn to counteract it. Societal Intervention: Educate each other and particularly our children at a younger age to understand implicit and learn to compensate for it, so that those who choose to work in health care don’t come with biases to be unlearned.
- Systemic or Socio/Cultural/Economic Factors. Different levels of income, family support, educational attainment, quality of housing, neighborhood safety may be associated with different demographic groups and be a major driver for unequal health outcomes. Example: Differential rates of obesity, hypertension and diabetes in different demographic groups, which lead to differential morbidity and mortality rates. Provider Intervention: Extra in-reach and out-reach activities, including addressing key social needs to have the health care team overcome the underlying socio-cultural factors and improve health care quality outcomes despite the underlying systemic factors. Societal Intervention: Support federal, state and local policies and interventions which reduce the underlying social and economic factors driving the difference.
- Supporting a Culture of Diversity, Equity, and Inclusion (DEI)in the workplace. Strictly speaking, activities to support DEI in the health care workplace are a societal-level intervention to reduce bias and inequities, but the ideals of DEI in a health care organization support that organization’s propensity to the meaningful interventions listed above. Examples: Designating someone in the health care organization’s leadership to spend time and energy focusing on equity; supporting an employee equity committee that reviews HR data, and practices for potential interventions.
PHC will follow DHCS’ lead and direction in using the the National Committee for Quality Assurance (NCQA) Health Equity Framework as a foundation for extending our previous work in population health/health equity to a new national standard. This new standard includes all three activities above: better measurement of disparities, focused and effective interventions to reduce/eliminate disparities, and activities to support DEI among our staff.
We encourage you to work toward improving health equity in these same three realms.
- Use data you have in your electronic systems to analyze disparities that you may be able to detect better than PHC, which now uses only county-provided demographic data usually self-declared in the Medi-Cal eligibility form.
- When you identify potential disparities either from the data analysis in step 1 or from direct feedback from patient complaints or feedback, evaluate options for how to reduce this disparity.
- Discuss any changes your company can make to support staff having a greater understanding of implicit bias, the historic roots of racism and other discrimination, and ways to compensate for this.
Finally, put your organization’s plan in writing and review it periodically at all-staff meetings, to keep the momentum in the right direction.
We all need to do our part to make our health care delivery system more equitable.
For more materials on health and racial equity, see the California Healthcare Foundation, the Center for Health Care Strategies, and Health Begins.