The national opioid epidemic along with the continued scourge of illicit narcotics, stimulants and alcohol has pushed regulators and policy makers to find community level solutions for these drugs and to expand drug rehabilitation services to an ever-growing population. The issue is the subject of much public discussion and attention. For instance, the California Health Care Foundation has made MAT a core component of their opioid reduction initiative (see the CHCF monograph, Recovery within Reach[1])
One result of the focus on opiate addiction is the Drug Addiction Treatment Act of 2000, which allows physicians of any specialty to be able to prescribe schedule III, IV and V opiates upon completion of an 8 hour program. Specialized providers are able to prescribe buprenorphine and naltrexone beyond the usual settings of methadone maintenance clinics. However, primary care based medication assisted treatment (MAT) services is the cornerstone for organizations and agencies addressing the opioid epidemic and in particular for the Medi-Cal population and Partnership HealthPlan. There are challenges and advantages for primary care physicians who provide medication-assisted treatment in their clinical practices. The challenges include a more complex population that may have (so far) not succeeded with other forms of addiction treatment including residential recovery programs or addiction counseling. Primary care physicians treat a variety of mild to moderate forms of chronic diseases such as hypertension, diabetes, and heart disease, and often refer those more serious patients for specialty care. Should such a model apply with substance use patients — can primary care physicians effectively treat patients with serious substance use disorders or should they be provided the referral resources that could more effectively address substance use problems?? Moreover, opioid users in MAT programs have much higher psychiatric co-morbidities making it even more difficult to effectively treat them in a primary care setting.
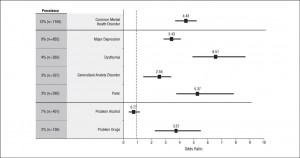
The table below suggests that the prevalence of common mental health disorders is up to 6x higher in opioid abusing populations. A recent national study has found that over 50% of all opioids are prescribed to individuals with a mental health diagnosis.[2] Finally, the MAT model can be labor-intensive with high frequency office visits requiring effective interpersonal communication, lab monitoring as well as prescription monitoring through Prescription Drug Monitoring Programs (PDMPs). (See below for a discussion of the pending Drug Medi-Cal model that could facilitate that handling of MAT in clinics). Primary care physicians are stretched in over-subscribed practices and increasing numbers of mandated activities and reporting. Adding MAT to this menu of work could lead to physician burn out without ensuring that a referral network is available.
There are significant advantages to locating medication assisted treatment in primary care practices — primarily continuity of care, family and support system orientation, and the psychosocial nature of primary care. Research has shown that recovery from addiction is significantly enhanced by family and peer support and individuals suffering from substance use often have chronic health conditions that also need to be addressed. Primary care clinicians, especially family physicians, care for patients throughout their life cycles, often from birth to death, through the stresses of adolescence and adulthood. Having this understanding not only of the patients medical history but also their psychosocial history, allows primary care physicians a more ready reservoir of knowledge of the drivers of substance use for particular patients. In addition to this, primary care physicians often treat not just the patient but the whole family as well as neighbors and friends. This enables the primary care physician to have a deeper understanding of what supports are present or need bolstering for the recovering patient. Finally, primary care physicians understand that substance use disorders are not cured by drugs alone. Developing a therapeutic relationship, connecting the patient to support resources, and monitoring the red flags of psychosocial distress are core competencies for many primary care clinicians. MAT is a natural fit into this practice design. A central caveat to this assertion is that primary care physicians cannot do the full gamut of MAT and substance use treatment without partners such as behavioral care specialties, social work and social agencies and addiction specialists.
The Drug Medi-Cal Program and SB 323.
In the coming years, the full continuum of substance use services will be available to PHC members, either through county run programs or through the “Regional Model” operated by PHC in other counties. Full details are available on our website. Through these programs, Medi-Cal will reimburse community primary care providers for the range of counseling, medication management, and social supports that are needed for effective MAT services. Of course, this requires a level of coordination and collaboration between DHCS certified MAT providers and other primary care community providers that will be essential as we move forward.
At this time, it is unclear how Federally Qualified Health Clinics, and Rural Health Clinics can most effectively participate in the Drug Medi-Cal Program. At the minimum, PHC will continue to pay providers for the administration of MAT and work to facilitate the necessary social supports. However, we are hoping for approval of SB 323, pending in the Legislature, which will specifically allow such clinics to be Drug Medi-Cal certified and participate in all aspects of the drug treatment system without endangering their prospective payment structure or facing adverse audit consequences.
To learn more about the Drug Medi-Cal Benefit, visit the PHC website at: http://www.partnershiphp.org/Providers/HealthServices/Pages/Drug%20Medi-Cal/Drug-Medi-Cal-Benefit.aspx or email drugmedicalphc@partnershiphp.org
By: Scott Endsley, MD (Associate Medical Director, Quality) Margaret Kisliuk (Behavioral Health Administrator)
[1] http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/PDF%20R/PDF%20RecoveryReachMAT.pdf
[2] Davis MA, Lin LA, Liu H,Sites BD. Prescription Opioid Use Among Adults with Mental health Disorders in the United States. J.Am Board Fam Med, 2017; 30: 407-417
